- Landers StratAGEy
- Posts
- #2 Shrinkflation in Home Health? Post Hospital Care Preferences
#2 Shrinkflation in Home Health? Post Hospital Care Preferences
Landers StratAGEy Newsletter #2 5/30/2024
Preference for Home Health
A surgical colleague who encouraged my work to improve home health services once told me in his pre-surgery office visits “Steve, my patients are more afraid of not being able to quickly go home after they leave the hospital than they are of the surgery itself.” I don’t know how often this is the case, and I’m certain there are patients who are more scared of going home without enough help and need/welcome the “all-inclusive” support of a high-quality rehabilitation or nursing facility. But, to add some data to the topic of post-hospital care preferences, late last month a group of researchers from Harvard University and the University of Rochester (including former MedPAC member Dr. David Grabowski) published an interesting new analysis on patient and caregiver preferences of post-hospital home health vs skilled nursing facility care.
In this unique “choice experiment” the researchers surveyed over 1500 potential patients and caregivers, and they concluded there was a high preference for home health, and the preference was so strong that the respondents were seemingly willing to pay out of pocket to make it happen. There are several other findings and nuances to the survey results, so I encourage anyone interested to review the full article. The JAMA Health Forum piece is titled Preferences for Postacute Care at Home vs Facilities, and the corresponding author is Fangli Geng.
Has Shrinkflation Come to Home Health?
Given public/patient preferences for home health, the potential for home health to be a cost-effective option, and the need to strengthen home and community care for a rapidly aging population—why would Medicare home health spending and Medicare home health visits be going down? Take a look at the charts below that really have me worried for homebound Medicare recipients.
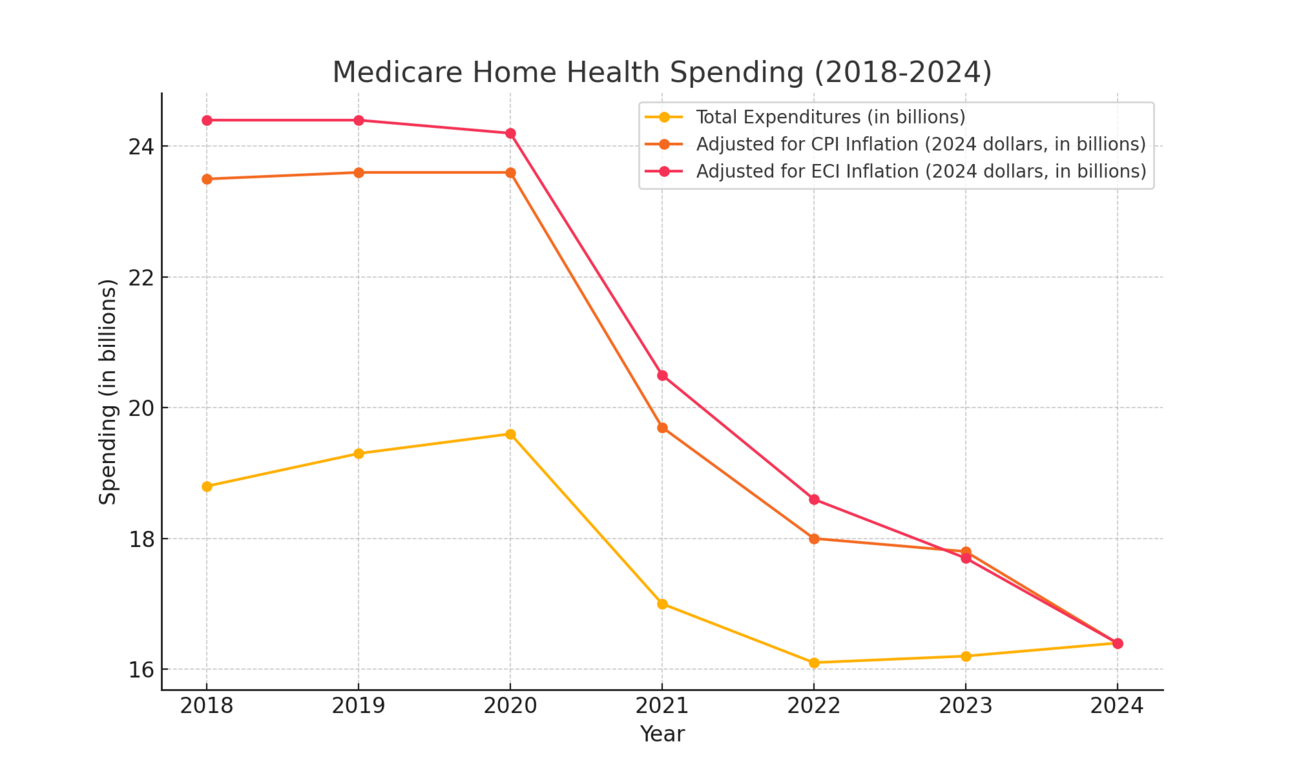
(Traditional / fee for service Medicare only, not adjusted for annual enrollment changes, ‘23 and ‘24 spending levels estimated from CMS rules, ECI adjustment uses healthcare and social assistance sector total compensation trends)
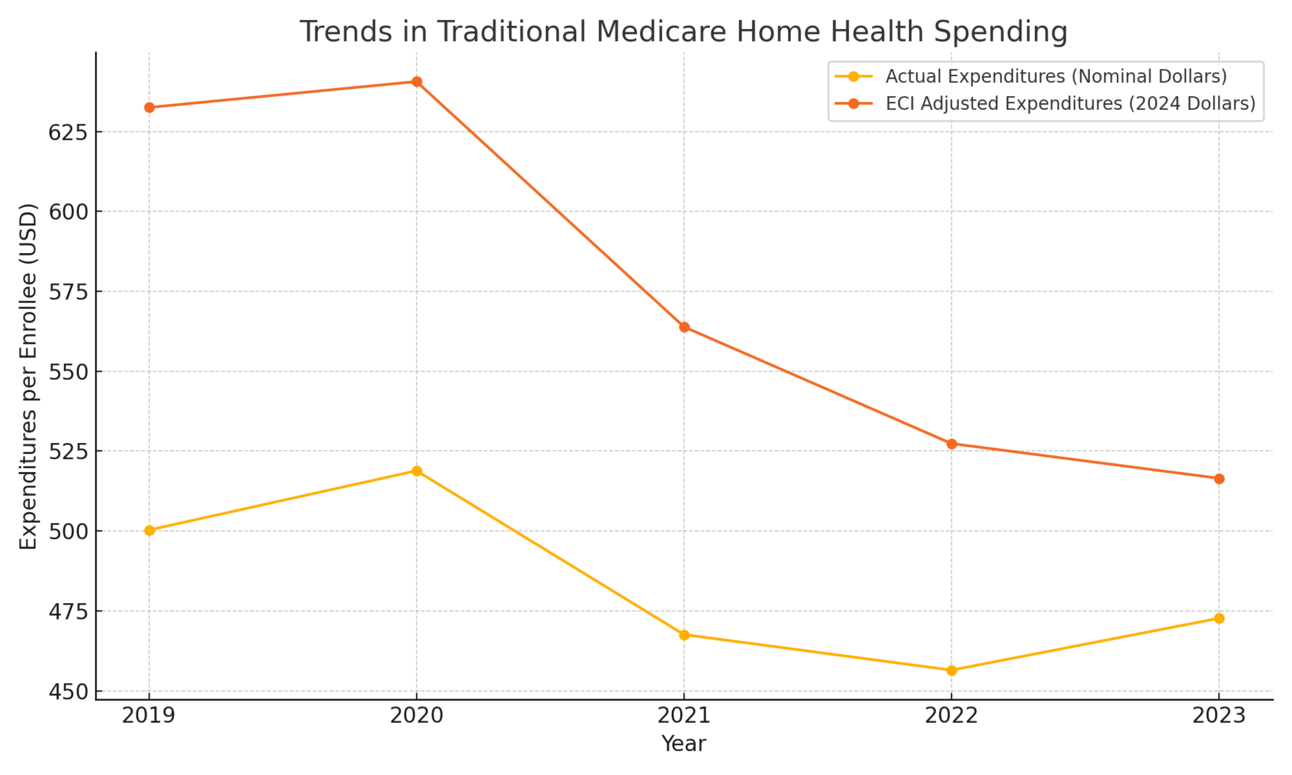
(Traditional / fee for service Medicare only, ‘23 spending levels estimated from CMS rule)
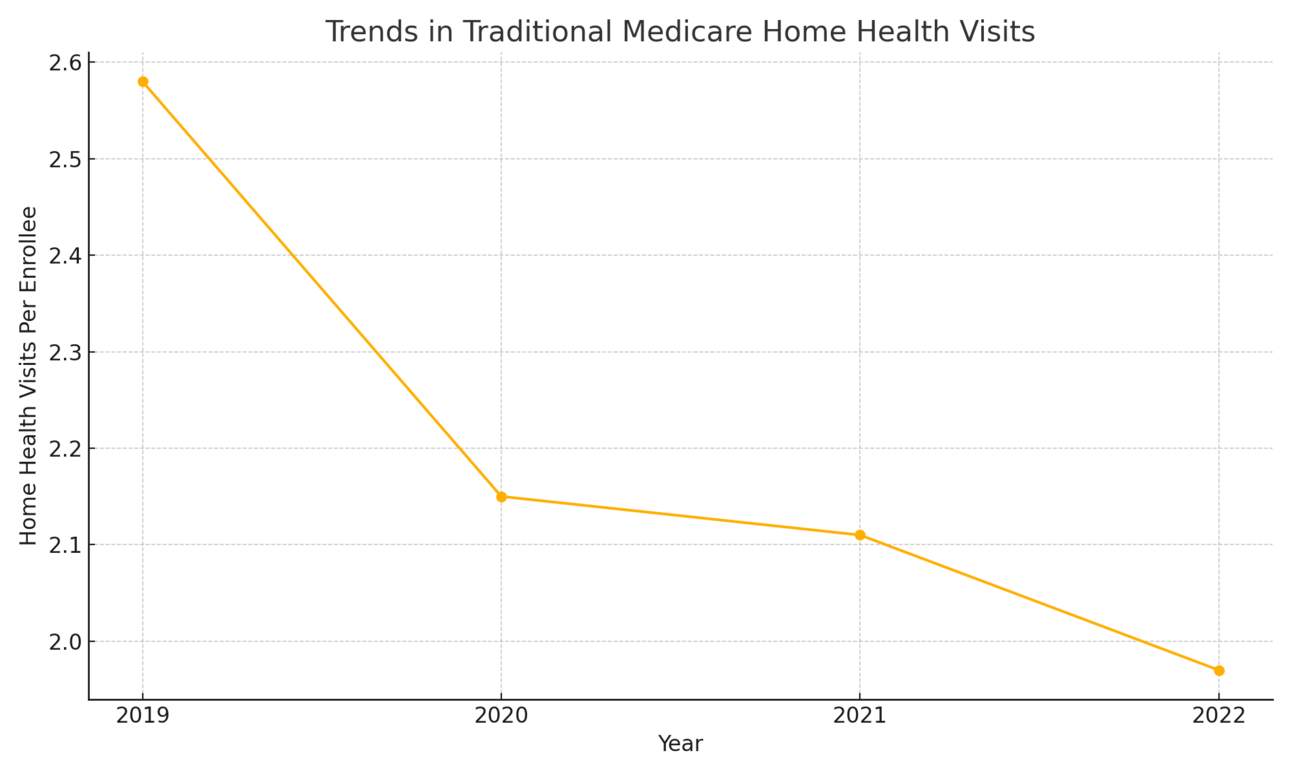
Traditional / Fee for Service Medicare Only
These charts have me concerned for the scary possibility of a depletion of resources, talent, and services available to help highly vulnerable people on Medicare. Understanding what is happening in these charts and “the why” behind the trends is a complex undertaking beyond the scope of this one newsletter. In short, I believe the trends are the results of: 1. Medicare home health policy changes that were implemented without any real-world testing to see how they would impact homebound seniors, 2. Reactive practice changes by home health agencies around how many visits they offer in response to the new payment policies, 3. Rapid wage and benefit cost inflation for the healthcare workforce (well deserved raises) may mean agencies can’t afford to offer as many visits, and 4) Medicare Advantage enrollment is outpacing Traditional Medicare enrollment, so the 1st graph above in-part reflects that trend (the other two are adjusted per enrollee)—by the way the overall picture of home health spending and access to care / visits in Medicare Advantage is basically a black box other than some insights we have from a few reports (some discussed in my last newsletter).
Could it be that these trends are to be cheered as the system becoming more efficient? A better deal for taxpayers? Less waste? It’s possible, but without a lot more information, I’m not ready to buy that. I’ve seen first-hand for my patients and parents the life changing impact of home health nursing and therapy visits—while I’m certainly aware of times when the need for certain home visits could be questioned as wasteful, more often in my experience these services are so important and there’s frequently a need for more—not less. What is happening to seniors and their families when we abruptly suck millions of visits and $billions in resources out of the home health system in such a short period of time?
My heart sinks when I think of people having more limited recovery or setbacks due to less therapy services, maybe they never get back to safely walking or climbing stairs. What about the person unnecessarily hospitalized when a few more nursing visits could have prevented it? And, sadly I fear the possibility of a family giving up on being able to keep mom or dad at home even when they promised it because there’s just not enough support and resources.
When we talk about Medicare policy, it’s easy to get tangled up in the complexities and all the competing demands, but I like to try and stay grounded in the impact on my parents and patients and how Medicare started in the first place. At the signing of the Medicare law in 1965 President Lyndon Johnson remarked that the law “…calls upon us never to be indifferent toward despair. It commands us never to turn away from helplessness. It directs us never to ignore or to spurn those who suffer untended in a land that is bursting with abundance.” Until proven otherwise, I’m concerned these home health trends could represent an increase in untended suffering for the oldest and sickest people on Medicare. There is nothing more basic and fundamental to a compassionate and effective healthcare system for an aging population than a robust and stable home health function. This isn’t the place to skimp. What is going on here? I reserve the right to have been wrong to worry as more information comes in, but the red flags are up.
